 The World Health Organization’s (WHO) “World Immunization Week 2025” lasted from April 24 to April 30, celebrating the 154 million lives vaccines have saved over the past 50 years. Governments and nongovernmental organizations (NGOs) have united in the mission to end preventable diseases and their efforts have already eradicated smallpox and nearly eradicated polio. Building on this momentum, several countries have successfully rolled out immunization campaigns in the past year alone. Here are four vaccines in developing countries that inspire hope for a healthier future.
The World Health Organization’s (WHO) “World Immunization Week 2025” lasted from April 24 to April 30, celebrating the 154 million lives vaccines have saved over the past 50 years. Governments and nongovernmental organizations (NGOs) have united in the mission to end preventable diseases and their efforts have already eradicated smallpox and nearly eradicated polio. Building on this momentum, several countries have successfully rolled out immunization campaigns in the past year alone. Here are four vaccines in developing countries that inspire hope for a healthier future.
Malaria Vaccine in Sudan
The Federal Ministry of Health (Sudan), the United Nations Children’s Fund (UNICEF), WHO and Gavi, the Vaccine Alliance partnered in November 2024 to distribute the first malaria vaccines in Sudan. Indeed, the country is the first in the WHO’s East Mediterranean region to introduce a vaccine for the disease.
Sudan has one of the highest rates of malaria infection in the region, with more than 1.3 million cases in 2023, of which 22.3% were children. Ongoing conflict has caused vaccination coverage to fall to 30% in active-conflict zones. However, the campaign distributed the vaccines to 15 health facilities and 148,000 children. The number of facilities will rise to 129 throughout 2025 and 2026.
Ebola Vaccine in Sierra Leone
Alongside Liberia and Guinea, Sierra Leone was one of the three countries most affected by the 2014 West Africa Ebola virus outbreak. However, it is the first of the three to introduce a nationwide preventive vaccine for the disease. The campaign began in December 2024 and administered the vaccine to 20,000 health care workers across 16 districts.
Health care workers carry a high risk of infection when treating the Ebola virus. Sierra Leone lost 7% of its health care workforce to the disease during the 2014 outbreak. The campaign follows a series of immunization successes in the country. It has also reached 90% diphtheria-tetanus-pertussis vaccine coverage since 2001 and 100% human papillomavirus (HPV) vaccine coverage as of September 2024. Sierra Leone shows that vaccines in developing countries can achieve and sustain results.
Vaccine Education in Trinidad and Tobago
The Pan American Health Organization (PAHO) led a two-day workshop for 79 school nurses in Trinidad and Tobago that covered how to talk to patients about vaccines and correct misconceptions. The country is emphasizing HPV vaccination, which can prevent 70% of cases of cervical cancer, for children 9–14 years old.
In Trinidad and Tobago, there are an estimated 202 women diagnosed with cervical cancer and 127 die from it every year. The nurses found the sessions informative and now have strategies to communicate the safety of vaccines to their patients. This signals a productive future for vaccines in developing countries.
Vaccines in Conflict-Affected Areas of Cameroon
In 2024, the Cameroon Baptist Convention Health Services (CBCHS) partnered with UNICEF to bring vaccines to conflict-affected northwest and southwest Cameroon areas. Non-State Armed Groups initially prevented the health care workers from entering the regions. However, Ful Morine Fuen of CBCHS persuaded them, saying they could not “kill diseases like malaria, diarrhea, etc. with a gun” but with vaccination.
The workers targeted displaced families, assessing the vaccination status of children aged 6 months to 5 years. They referred children needing vaccines to local facilities or administered vaccines through mobile clinics. Twelve families were hesitant about vaccination, but 11 of them agreed to it after workers discussed the benefits. In total, 473 children received the necessary vaccines.
Looking Ahead
Vaccines in developing countries have helped thousands of people in the past year. The continued efforts of local governments and international health organizations will stop the spread of preventable diseases. They will save even more lives by World Immunization Week 2026.
– Tyler Payne
Tyler is based in Allentown, PA, USA and focuses on Global Health and Politics for The Borgen Project.
Photo: Flickr

 On July 4, 2022, the Democratic Republic of the Congo’s Ministry of Health announced the
On July 4, 2022, the Democratic Republic of the Congo’s Ministry of Health announced the 
 In recent years, studies have shown that Information and Communication Technologies (ICTs) have proven to be helpful for vulnerable communities on many different fronts. Since the start of the COVID-19 pandemic, it has been observed that women have increasingly used ICTs, especially those in developing countries.
In recent years, studies have shown that Information and Communication Technologies (ICTs) have proven to be helpful for vulnerable communities on many different fronts. Since the start of the COVID-19 pandemic, it has been observed that women have increasingly used ICTs, especially those in developing countries.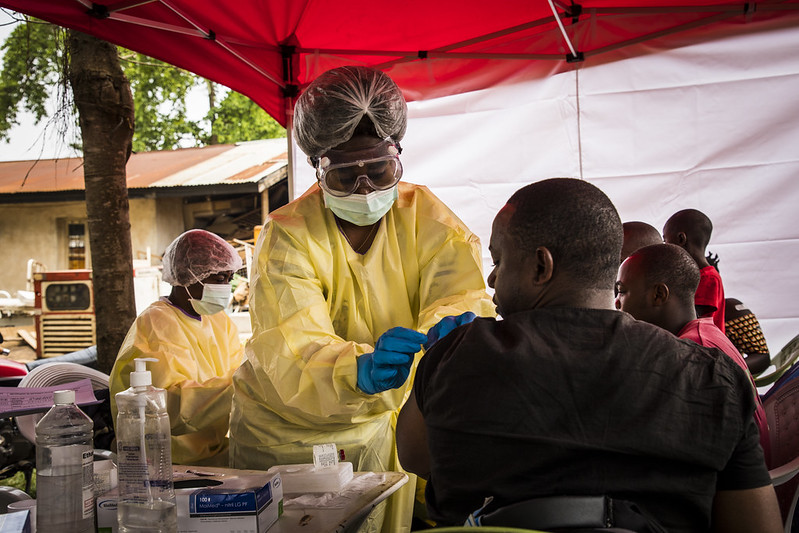 The Ebola Virus Disease (EVD) has ravaged countries in sub-Saharan Africa since its identification in 1976. Overall, there have been
The Ebola Virus Disease (EVD) has ravaged countries in sub-Saharan Africa since its identification in 1976. Overall, there have been  Many important improvements in educational outcomes have occurred in Sierra Leone since 2015, especially for women and children. The country is bouncing back from the civil war, Ebola crisis and other serious challenges. This progress is partially owed to organizations that help children go to school. Several NGOs and community-based actors support education in Sierra Leone. Here is a small glimpse into the work of many.
Many important improvements in educational outcomes have occurred in Sierra Leone since 2015, especially for women and children. The country is bouncing back from the civil war, Ebola crisis and other serious challenges. This progress is partially owed to organizations that help children go to school. Several NGOs and community-based actors support education in Sierra Leone. Here is a small glimpse into the work of many.

 Sierra Leone is a West African country bordered by the North Atlantic Ocean. It is an impoverished country with almost half of the working-age population involved in subsistence agriculture. Between 1991 and 2002, Sierra Leone was
Sierra Leone is a West African country bordered by the North Atlantic Ocean. It is an impoverished country with almost half of the working-age population involved in subsistence agriculture. Between 1991 and 2002, Sierra Leone was 