The presence of the malaria epidemic in the developing world has decreased significantly. However, for specific populations, malaria is still a life-threatening disease. There is a strong demand and need to prevent and treat malaria in pregnancy.
Malaria poses a threat to pregnant women and contributes to both maternal and infant mortality. In addition, malaria during pregnancy can result in maternal anemia and low birth weight of children. Stillbirths, miscarriages and preterm births are associated with malaria in pregnant women.
Given these facts, malaria poses a risk to communities and families, particularly when pregnant women contract the disease.
In Sub-Saharan Africa, malaria in pregnancy is associated with Plasmodium falciparum infection, but can also result from Plasmodium vivax.
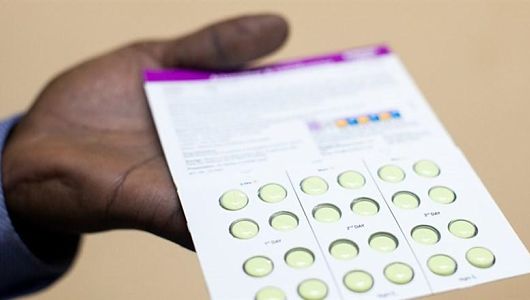
Current strategies to address malaria in pregnancy include intermittent preventive treatment with sulfadoxine-pyrimethamine, use of insecticide-treated nets and treatment if malaria is contracted.
Pregnant women in the developing world have had difficulty receiving necessary health care due to inefficiencies within health care systems and lack of awareness about specialized treatment.
Local staff may not have the training or resources to offer pregnant women. In addition, preventive sulfadoxine-pyrimethamine and insecticide-treated nets are not widely available. There is a lack of skill and the ability to scale up the resources that are available.
Moving forward, malaria treatment for pregnant women would likely be more successful if policies and programs could work with other maternal and reproductive health programs.
Clara Menéndez, a medical researcher at ISGlobal, and her colleagues emphasize that a multidisciplinary approach will be required to fully address malaria and how it impacts the lives of pregnant women and their families.
– Iliana Lang
Sources: The American Journal of Tropical Medicine and Hygiene, The Lancet Global Health The London School of Hygiene and Tropical Medicine
Photo: 100X Development Foundation
 Every minute, a child dies from malaria. 90 percent of the deaths from malaria occur in the poorest African countries. Malaria is a preventable, treatable disease, yet more than half of the world’s population continues to be at risk.
Every minute, a child dies from malaria. 90 percent of the deaths from malaria occur in the poorest African countries. Malaria is a preventable, treatable disease, yet more than half of the world’s population continues to be at risk.