Mere weeks after the confirmation of the first ten cases of poliomyelitis in Syria, Mother Nature dealt the global health community another powerful blow in the form of Typhoon Haiyan.
Some areas of the Philippines are nearly 95 percent destroyed; Doctors Without Borders staff has described the aftermath as reminiscent of the Haitian earthquake of 2010. Hospitals have been ruined, so aid workers have set up temporary health centers to treat wounds and provide much-needed vaccines to locals and returning residents who chose to flee the oncoming storm.
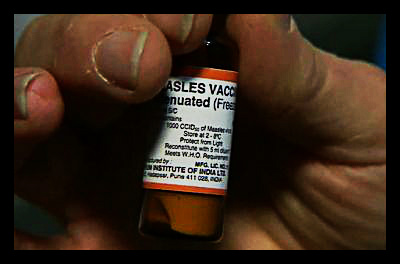
The World Health Organization and the Philippine Department of Health have spearheaded a campaign to vaccinate children under five against measles or polio outbreaks and provide Vitamin A drops to boost immune system strength. All children under 15 years will then receive care if resources allow. Hard-hit areas are the campaign’s priority. Immediate needs include the set-up of immunization stations, volunteer deployment and acquisition of all necessary vaccines.
Philippine Secretary of Health Enrique Ona guarantees that since “system is shaken but not broken,” a re-launch of widespread vaccinations should not prove impossible.
Nonetheless, in some regions such as Guiuan (to the east of Samar island,) the “cold chain” required for vaccine delivery and preservation has not yet been implemented. This mechanism involves gas and generator powered refrigerators, cold boxes, ice packs and vaccine-cases for areas without power. In the words of Dr. Johan von Schreeb of Doctors Without Borders, the devastated islands “do not have time to wait.”
This refrigeration conundrum arises with each civil conflict or natural disaster that leaves affected regions without power. Though the cold chain concept is effective and familiar to health care providers, current supply and logistics systems were designed thirty years ago, prior to the development of cold chain equipment. Project Optimize (a task force of the WHO and PATH) and UNICEF’s Cold Chain and Logistics Task Force have identified innovative funding for cold chain equipment as a key opportunity for improvement upon today’s vaccine systems.
In order to achieve the Project’s 2020 goals, cold chain equipment, efficiency and monitoring must improve. Health care managers must be able to access performance figures to make informed purchasing and allocation decisions given the limited time span and resources available in health care emergencies; in other words, the current Philippine situation. If local or national health departments allot too many or too few resources to any single immunization station, lives will be lost (due either to a vaccine shortage or to spoliation of vaccines that should have been administered in other areas). Striking this delicate balance requires widespread cooperation between the public and private sector.
Similarly, manufacturers of equipment must be kept abreast of product performance in the field. The implementation of a feedback loop between manufacturer and user would improve product packaging and design. The Project’s 2013 Action Plan suggests beginning with a redesign of cold boxes to maximize the “refrigerant-to-vaccine” ratio to hold more vaccines and insulate them more efficiently.
Improvements to vaccine logistics that reflect needs expressed explicitly by those on the front lines of vaccine campaigns will ensure that doctors such as von Schreeb have the tools to work their magic when disaster strikes.
– Casey Ernstes
Sources: Doctors Without Borders, PATH, The World Health Organization, The World Health Organization
Photo: BBC







