 Guinea is a country in West Africa bordered by the Atlantic Ocean. It is home to nature reserves that hold a forested mountain range rich with native plants and animals. However, despite this preserved nature, the people of Guinea lack basic living standards. About three-quarters of the Guinea population experience extreme poverty. They have a lack of education, health care and hygiene. This lack of adequate health care has made Guinea home to many diseases. These diseases, specifically lower-respiratory infections are the cause of 99.9% of deaths in the country. The prices of health care and the low amounts of health professionals per population are the main causes of the lack of adequate health care. However, significant improvements have been made through initiatives by the USAID to improve the quality of health care.
Guinea is a country in West Africa bordered by the Atlantic Ocean. It is home to nature reserves that hold a forested mountain range rich with native plants and animals. However, despite this preserved nature, the people of Guinea lack basic living standards. About three-quarters of the Guinea population experience extreme poverty. They have a lack of education, health care and hygiene. This lack of adequate health care has made Guinea home to many diseases. These diseases, specifically lower-respiratory infections are the cause of 99.9% of deaths in the country. The prices of health care and the low amounts of health professionals per population are the main causes of the lack of adequate health care. However, significant improvements have been made through initiatives by the USAID to improve the quality of health care.
Disease Prevalence in Guinea
Guinea hosts all kinds of diseases, both communicable and noncommunicable and some endemic diseases. The most prevalent diseases within Guinea are Malaria, HIV/AIDS, Tuberculosis and Neglected Tropical diseases. There are 4.5 million cases of Malaria a year which caused 9,439 deaths in 2021. Tuberculosis and HIV/AIDS affect every 175 in 10,000 people. Though they have treatments and detection systems it is hard for these to operate in Guinea due to the low coverage of Tuberculosis services, human resources shortages and lack of follow-ups among patients. Many Neglected Tropical Diseases such as Leprosy, Rabies, Buruli ulcer, foodborne trematodes and many more are also prevalent within the region.
Immunization Challenges and Systematic Issues
Another area besides diseases that cause poor health practices for the Guinean people is the lack of immunization. Many children are zero-dose children meaning they have never had a vaccine in their life. Only 24% of the 192,000 children born each year receive a complete cycle of vaccinations. This leads to the furtherance of these preventable diseases and causes endemics.
Evolution of Guinea’s Health Care System
Between 1986 and 1989, the privatization of health care began to grow in Guinea, ultimately raising the cost of care and making it inaccessible to the majority of the population. Currently, health care remains expensive and the quality of care is unsatisfactory. As of 2008, only 5% of the population had coverage under public health insurance. Guinea’s health care system has a pyramidal structure, featuring three national hospitals, one regional hospital in each of the seven regions and a prefectural hospital in each of the 33 prefectures. Despite the seemingly comprehensive system, there is a critical shortage of health care workers. The distribution of these workers is also uneven: 60% of health care workers are located in Conakry, the capital, which is home to only 20% of the population. Consequently, Guinea’s health care system suffers from a severe lack of accessible care and health care professionals.
Launch of Notre Sante Initiative by USAID
Notre Sante or “Our Health”, is a USAID initiative launched in June 2023 to provide accessible, affordable and high-quality health care in Guinea. The project aims to operate across 15 prefectures in the regions of Labé, Boké and Kindia, as well as the six communes of Conakry. It plans to collaborate with the Ministry of Health and Public Hygiene and engage both private and public sectors. Notre Sante focuses on improving provider behavior and delivering care in a culturally sensitive manner that involves community members and builds on best practices. The launch of this initiative marks significant progress toward enhancing health care for the people of Guinea.
Future Prospects for Health Care in Guinea
Guinea’s health care system has struggled with inadequate services and a shortage of health care professionals. However, the introduction of the Notre Sante initiative offers hope for improving the quality of life for the people of Guinea. Notre Sante aims to make health care affordable, accessible and high-quality, signaling a hopeful future for the trajectory of Guinea’s health care system.
– Ellie Buss
Ellie is based in Vancouver, WA, USA and focuses on Good News and Global Health for The Borgen Project.
Photo: Flickr

 Since launching the
Since launching the  AIDS (acquired immunodeficiency syndrome) is a highly stigmatized disease. Throughout history, the AIDS epidemic has brought on severe discrimination toward individuals on the basis of race, sexual orientation and socioeconomic status. The epidemic
AIDS (acquired immunodeficiency syndrome) is a highly stigmatized disease. Throughout history, the AIDS epidemic has brought on severe discrimination toward individuals on the basis of race, sexual orientation and socioeconomic status. The epidemic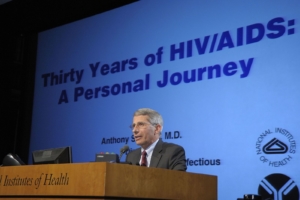 The 24th Annual AIDS conference occurred in Montreal between July 29, 2022 and August 2, 2022. This was the first year the conference employed a hybrid model with both in-person and virtual speakers. As a result, researchers, advocates and leaders from
The 24th Annual AIDS conference occurred in Montreal between July 29, 2022 and August 2, 2022. This was the first year the conference employed a hybrid model with both in-person and virtual speakers. As a result, researchers, advocates and leaders from  Malaysia saw its first confirmed case of COVID-19 on January 24, 2020. The Malaysian government implemented the Movement Control Order (MCO or PKP) around two months later in response. This mandate restricted travel, work, assembly and established quarantine measures jeopardizing the financial integrity of Malaysian households. Here is some information about the impact of COVID-19 on poverty in Malaysia as well as the country as a whole.
Malaysia saw its first confirmed case of COVID-19 on January 24, 2020. The Malaysian government implemented the Movement Control Order (MCO or PKP) around two months later in response. This mandate restricted travel, work, assembly and established quarantine measures jeopardizing the financial integrity of Malaysian households. Here is some information about the impact of COVID-19 on poverty in Malaysia as well as the country as a whole. Since the early 2000s, Afghanistan’s disease prevention and
Since the early 2000s, Afghanistan’s disease prevention and  On May 12, 2022, the president of North Korea,
On May 12, 2022, the president of North Korea, 

