For years, many issues have plagued Uganda’s health care system. The vast majority of its population lives in rural areas with limited access to health care. Medical professionals are scarce, and their services are often extremely expensive. However, amid these challenges, a solution has emerged: mobile health technology. These innovative platforms connect users with essential healthcare services and provide access to incredible tools through personal devices. Mobile health technology in Uganda is laying a strong foundation for a more equitable future.
For years, many issues have plagued Uganda’s health care system. The vast majority of its population lives in rural areas with limited access to health care. Medical professionals are scarce, and their services are often extremely expensive. However, amid these challenges, a solution has emerged: mobile health technology. These innovative platforms connect users with essential healthcare services and provide access to incredible tools through personal devices. Mobile health technology in Uganda is laying a strong foundation for a more equitable future.
Struggles of the Past
The country has one of the worst doctor-to-patient ratios in the entire world. There is roughly one doctor for every 25,000 citizens. This falls drastically short of the World Health Organization’s (WHO) recommendation, which is to have one doctor for every 1,000 people.
Health care in Uganda is largely unaffordable. Brown University’s Kyoko Saito recently traveled to Uganda, where she noted that one night in the hospital costs around $20, a shocking figure when considering that the country’s average monthly income is $78. Furthermore, hospital staff determine whether or not patients are financially stable and turn them away if they cannot pay for treatment.
Ugandan health systems struggle to obtain and restock essential equipment, store reliable health information and ensure quality of overall service.
Put simply, the fundamental structure of the Ugandan health care system is broken. There are not enough resources and not enough medical professionals. Furthermore, to exacerbate the issue, health care is expensive and predominantly located in urban areas, alienating around 70% of the rural population.
What is Mobile Health Technology?
Mobile health technology, commonly referred to as mHealth, is an umbrella term for the use of mobile phones and other personal electronic devices in medical care. Potential uses for mHealth include:
- Tracking medical data and storing digital records
- Enhancing communication between doctors and patients with secure messaging channels
- Offering virtual training programs for essential workers
- Allowing doctors to evaluate, diagnose and treat patients remotely through video consultation, imaging reports, e-prescriptions, etc.
- Managing chronic diseases through mobile apps
- Implementing nutrition monitoring systems
Although mHealth has only been around for a few years, 83% of physicians in the U.S. already use it to provide care. Expanding mobile health technology in underdeveloped countries like Uganda will lead to further benefits.
mHealth in Uganda
Currently, almost 30% of Ugandans have access to the internet, and this figure grows rapidly each year. The increased dissemination of electronics in recent years has allowed for mobile health technology in Uganda to flourish, working to address the fundamental issues that plague its health care system. Here are a few examples of the uses of mobile health technology in Uganda:
- EVA System: A “mobile, AI-ready colscope that expands expertise on point-of-care cervical cancer screenings and sexual assault forensic examination.”
- Palliative Care: For patients with cancer who have limited access to in-person physicians, mHealth technology has shown incredible potential in providing necessary palliative care.
- Smart Health App: Stores patient data, plans for virtual appointments, provides instructions for care relating to immunization, childhood disease, pregnancy and more.
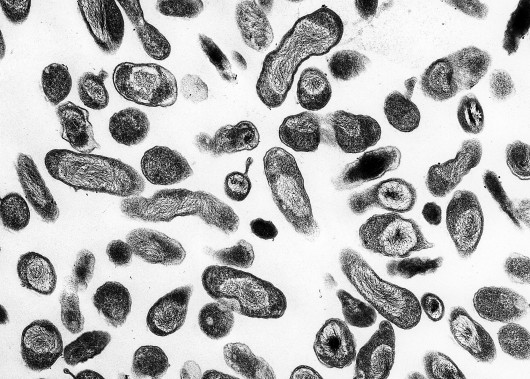
- Test Results: In southwestern Uganda, health workers utilized text messaging as a means of quickly transmitting results for HIV-positive citizens.
- Mass Communication: In northern and eastern Uganda, public health officials used text messaging to raise awareness for malaria and to remind patients to take their medication.
Looking Towards the Future
Mobile health technology in Uganda presents an inspiring solution that provides accessible, affordable health care to its citizens. Indeed, with these advancements, individuals in rural areas can now connect with medical professionals. Furthermore, hospitals can spend less on equipment and doctors can become less burdened by the vast overflow of Ugandans that need care. While there are significant hurdles that remain (namely, improving access to technology in rural areas of the country), the results have been extremely promising so far.
Over the next five years, Uganda’s mission will be to provide mobile health technology to over half of its inhabitants. This could ensure that the population can stay healthier (especially those in underfunded, remote locations), working to break the decades-long cycle of poverty that has affected millions of Ugandan citizens.
– Josh Weinstein
Josh is based in Chester Springs, PA, USA and focuses on Technology and Solutions for The Borgen Project.
Photo: Flickr

 Some of the largest barriers to HIV treatment and prevention in rural areas are access to care and affordability. Luckily, telehealth technology can help provide people in more isolated areas with access to information about HIV prevention and treatment. For individuals without a car whose nearest health center is 15 or more miles away, HIV-focused telehealth or telemedicine is a potential solution.
Some of the largest barriers to HIV treatment and prevention in rural areas are access to care and affordability. Luckily, telehealth technology can help provide people in more isolated areas with access to information about HIV prevention and treatment. For individuals without a car whose nearest health center is 15 or more miles away, HIV-focused telehealth or telemedicine is a potential solution.