 Nigerians have faced a growing crisis in health care access in recent years. Nigeria has a population of more than 200 million people, marking it as one of the most populated countries in 2024. The country has a diverse group of people, cultures and languages. Although the country has a huge potential for widespread affluence due to its oil and natural resources, its systems are lacking in meeting the needs of all its citizens. For its health care system, as of 2023, Nigeria was ranked 157th out of 167 countries. Improvement within the system is essential for the well-being of the Nigerian people to be guaranteed.
Nigerians have faced a growing crisis in health care access in recent years. Nigeria has a population of more than 200 million people, marking it as one of the most populated countries in 2024. The country has a diverse group of people, cultures and languages. Although the country has a huge potential for widespread affluence due to its oil and natural resources, its systems are lacking in meeting the needs of all its citizens. For its health care system, as of 2023, Nigeria was ranked 157th out of 167 countries. Improvement within the system is essential for the well-being of the Nigerian people to be guaranteed.
Malaria
Malaria is a life-threatening disease found in primarily tropical countries and is transmitted to humans by mosquitoes. In 2021, approximately 619,000 people died from malaria, with more than half of all malaria deaths worldwide occurring in four African countries. Nigeria’s health indicators are some of the worst in Africa. Nigeria continues to undertake the highest level of malaria cases globally, which is the leading cause of child illness and death. Professor Olubenga A. Mokuolu oversees all malaria work in the country.
In an interview, he gave one reason for Nigeria’s high malaria burden: the country’s environmental management. “In terms of environmental management, Nigeria leaves a lot to be desired. The country has open refuse sites and blocked drainage systems and because people lack piped water, they store water at home in containers. These all provide ideal sites for mosquitoes to breed.” While the number of malaria cases has gone down in recent years, they are not at a level where people can fully be at ease.
Lack of Access
Health care access in Nigeria is very limited due to factors within the health system. The Nigerian primary health care (PHC) system is the lowest level and entry point for Nigerians to receive health care services such as visitations, preventative, curative and rehabilitative services. Although initially, the PHC system was seen as a guiding policy for further health improvements, there were many flaws with its enactment.
Vivien O. Abah, a Nigerian health care researcher, stated that “The PHC system was deployed to the grassroots, but geographical access did not translate to access to health care as the populations did not utilize the majority (80%) of these facilities.” Not only was the lack of geographical access difficult but the quality of care in these primary health facilities was proven difficult for some as well.
What Is Being Done
The Nigerian health care industry has faced serious setbacks in recent years due to a lack of funding, as well as the mismanagement of creating accessible quality care for the population. This does not mean that the country has given up, as there have been various measures taken into consideration to improve the system.
In 2018, the government approved the second National Strategic Health Development Plan (SHDP), which sought to ensure all Nigerians have access to health care in the country, with a focus on preventing the trend of citizens traveling abroad for medical care. The Former President of Nigeria, Muhammadu Buhari, said that the SHDP will be a transparent and accountable mechanism implemented to ensure the health of all citizens and to forbid corruption from affecting funding.
The government has also focused on individual epidemics and issues that have affected Nigerians, as its preventative measures for malaria have saved tens of thousands of lives, most of them children. The country’s health care system provides more than 25 million children aged less than 5 with preventive chemotherapy for malaria, which has considerably reduced the children’s mortality rates.
Improving Health
Improvement of the Nigerian health care system will be a long and arduous process. and its efficiency highly depends on whether or not the government prioritizes high-quality care and population outcomes. In the past, people have had tremendous trouble seeking high-quality care, with some having to leave the country to receive treatment.
Health care in Nigeria has undergone significant changes and is moving in the right direction, but there is still progress to be made. With a growing population in a country known for diseases and limited medical access, the health care system cannot currently guarantee treatment for all its citizens.
– Oliver Martin
Oliver is based in Honolulu, HI, USA and focuses on Global Health for The Borgen Project.
Photo: Pixabay

 Mosquitoes play dual roles in ecosystems worldwide as major pollinators and a key food source. They also spread life-threatening diseases such as
Mosquitoes play dual roles in ecosystems worldwide as major pollinators and a key food source. They also spread life-threatening diseases such as 

 In 2022, more than 40% of countries experienced malaria outbreaks, resulting in approximately
In 2022, more than 40% of countries experienced malaria outbreaks, resulting in approximately  In January 2024, the World Health Organization (WHO) certified Cabo Verde as malaria-free, making it the
In January 2024, the World Health Organization (WHO) certified Cabo Verde as malaria-free, making it the  For Uganda, a country in East Africa, health is a major concern. Uganda’s population of 47 million has always been heavily impacted by illness and disease, with communicable diseases accounting for over 50% of deaths in the country. Malaria, tuberculosis (TB) and HIV/AIDS are three of the top diseases impacting Uganda and are among the leading causes of death.
For Uganda, a country in East Africa, health is a major concern. Uganda’s population of 47 million has always been heavily impacted by illness and disease, with communicable diseases accounting for over 50% of deaths in the country. Malaria, tuberculosis (TB) and HIV/AIDS are three of the top diseases impacting Uganda and are among the leading causes of death.  As one of the poorest countries in the world, Comoros experiences numerous challenges. This is exacerbated by the country’s history of political instability and a devastating socioeconomic climate. Poor health care has both a dramatic effect on the lifespan of Comorians and on their quality of life.
As one of the poorest countries in the world, Comoros experiences numerous challenges. This is exacerbated by the country’s history of political instability and a devastating socioeconomic climate. Poor health care has both a dramatic effect on the lifespan of Comorians and on their quality of life.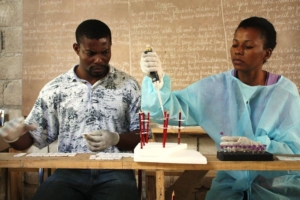 In October 2021, the World Health Organization (WHO) recommended a vaccine for the prevention of malaria. This malaria vaccine,
In October 2021, the World Health Organization (WHO) recommended a vaccine for the prevention of malaria. This malaria vaccine,  With a population of about 30 million, many Angolans do not have access to adequate healthcare. The limited access to quality healthcare is due to decreased funding due to the Angolan Government’s budget restrictions. The lack of funding affects the quality of public healthcare which people can
With a population of about 30 million, many Angolans do not have access to adequate healthcare. The limited access to quality healthcare is due to decreased funding due to the Angolan Government’s budget restrictions. The lack of funding affects the quality of public healthcare which people can