 More than two decades ago, Bill and Melinda Gates learned about the contagious Rotavirus, present in several countries. The more they learned, the more devoted they became to helping. Higher-income countries could treat rotavirus with ease, but lower-income countries struggled with it, leading to many casualties. Hearing this, the Bill and Melinda Gates Foundation started working in India in 2003. The foundation launched the Avahan Program, which targeted HIV prevention. Avahan was incredibly successful in its endeavors, eliminating nearly 600,000 infections.
More than two decades ago, Bill and Melinda Gates learned about the contagious Rotavirus, present in several countries. The more they learned, the more devoted they became to helping. Higher-income countries could treat rotavirus with ease, but lower-income countries struggled with it, leading to many casualties. Hearing this, the Bill and Melinda Gates Foundation started working in India in 2003. The foundation launched the Avahan Program, which targeted HIV prevention. Avahan was incredibly successful in its endeavors, eliminating nearly 600,000 infections.
The Bill and Melinda Gates Foundation also partnered with others to help the Indian government in defacing polio. These efforts were not easy; nearly 2.3 million volunteers helped with vaccination efforts, and their labors were fruitful. The efforts helped provide vaccines to 170 million children finally eradicating polio in India in 2014, according to the foundation’s website.
CDC in India
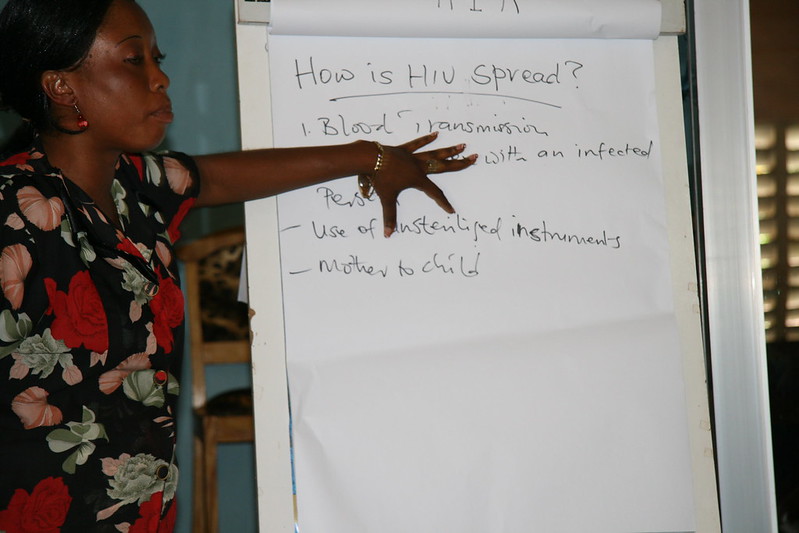
In 2001, the Centers for Disease Control and Prevention (CDC) established its first Indian office in New Delhi. Establishing this office was one of the first steps to their end goal: eliminating any presence of HIV in India by 2030.
The CDC, partnering with National AIDS Control Organization (NACO) began advancing HIV treatment in India. They improved accessibility to antiretroviral therapy (ART) and viral load (VL) testing. With CDC, NACO created 740 ART centers in India, all providing specialized care, disease management and ART, according to a 2024 CDC report.
Regarding their laboratories, the CDC has worked on reaching remote areas through community-led testing, and access to PLHIV. Additionally, the CDC is collaborating with the Indian Government to create systems within their laboratories, dedicated to the early detection and management of HIV, along with continued care regarding cervical cancer, according to the same report.
The CDC and the Indian Government have partnered together regarding testing, targeting districts with a high HIV prevalence, including Mumbai, Mizoram, Manipur, Nagaland, and Andhra Pradesh, according to the CDC. This partnership has led to an increased awareness and understanding regarding HIV.
USAID Project
Additionally, USAID and the Johns Hopkins University School of Medicine started a project to make HIV treatment available in socially remote areas. This program has opened several centers that help with treatment. There are centers dedicated to teenagers, where they have access to “sports, music, and life-skills programs, while also accessing counselling, social services and peer support on their HIV journey.”
This mix of services allows them to navigate life and challenges as they live with HIV. There are also centers for transgender people, that provide specialized treatment for HIV along with general healthcare services as well. In these specific centers, they provide stigma-free care, allowing for a more accepting, safe atmosphere for patients. There are also online platforms such as SafeZindagi.in, which can often be a faster or easier option for patients. It provides confidential care and counselling for those living with HIV.
HIV in India: The Future
Having centers like these available to the general public is a game-changer. Factors that may inhibit people from seeking care include stigma, transportation accessibility, cost, lack of awareness, and more. Programs like these, along with the work from the CDC and Indian government, are slowly tackling these issues and working towards a healthier India.
Now, around 2.5 million people are living with HIV in India, compared to the 39.9 million people living globally with HIV. Thanks to the efforts from the CDC, the Indian Government and USAID, HIV prevention in India is advancing in an upward trajectory.
– Lakshya Anand
Lakshya is based in Bellevue, WA, USA and focuses on Global Health for The Borgen Project.
Photo: Unsplash



 Singapore is a country at the tip of the Malaysian peninsula in Southeast Asia. The country
Singapore is a country at the tip of the Malaysian peninsula in Southeast Asia. The country  The quicker the response to a medical epidemic the better. This proved to be the case for Moldova in their response to the HIV/AIDS epidemic. An effective response is one to be learned, repeated and implemented for future use.
The quicker the response to a medical epidemic the better. This proved to be the case for Moldova in their response to the HIV/AIDS epidemic. An effective response is one to be learned, repeated and implemented for future use.

 Despite recent reductions in transmission rates of HIV/AIDS in Sierra Leone, the lack of knowledge and stigmatism surrounding the condition, particularly among the younger population, could prevent the country from further minimizing the spread of the disease.
Despite recent reductions in transmission rates of HIV/AIDS in Sierra Leone, the lack of knowledge and stigmatism surrounding the condition, particularly among the younger population, could prevent the country from further minimizing the spread of the disease. With a series of economic and political crises throughout the past decade,
With a series of economic and political crises throughout the past decade, 