 In October 2025, the World Health Organization (WHO) announced that the Maldives’ historic triple elimination of mother-to-child transmission of Human Immunodeficiency Virus (HIV), syphilis and hepatitis B had been officially validated. This certification makes the Maldives the first country in the world to successfully eliminate the transmission of all three life-threatening diseases from mother to child simultaneously. The milestone represents a major triumph for maternal health and provides a clear strategy for other low- and middle-income countries (LMICs) to follow.
In October 2025, the World Health Organization (WHO) announced that the Maldives’ historic triple elimination of mother-to-child transmission of Human Immunodeficiency Virus (HIV), syphilis and hepatitis B had been officially validated. This certification makes the Maldives the first country in the world to successfully eliminate the transmission of all three life-threatening diseases from mother to child simultaneously. The milestone represents a major triumph for maternal health and provides a clear strategy for other low- and middle-income countries (LMICs) to follow.
Understanding Triple Elimination
Triple elimination is a public health standard that ensures the next generation is born free of three specific infections that often cause lifelong health complications or infant mortality. To achieve this, the Maldives had to meet rigorous WHO criteria, including maintaining antenatal care coverage and testing rates above 95%. The nation also proved that its newborn interventions, such as the hepatitis B birth dose, are consistently delivered within 24 hours of birth. Data show that the Maldives recorded zero babies born with HIV or syphilis in both 2022 and 2023. Additionally, a national survey in 2023 confirmed that no young children entering school carried hepatitis B.
A Decentralized Approach to Maternal Care
Progress toward the Maldives’ historic triple elimination was made possible by a decade of systemic reform focused on reaching people in remote areas. Because the population is dispersed across more than 1,000 islands, the government prioritized a decentralized, community-based health care system. In 2018, the nation implemented the “Agenda for Integrated Service Delivery,” which standardized data collection for all three diseases. This ensured that even on the smallest islands, pregnant women could access free testing and treatment. By removing financial barriers, the government addressed a primary cause of health vulnerability among low-income families.
The Role of WHO and United Nations Children’s Fund (UNICEF)
The WHO and UNICEF played essential roles in supporting the Maldives during the validation process. The WHO provided the technical framework and training to ensure that screening and vaccination programs were integrated into routine maternal and child health services. UNICEF South Asia contributed by reviewing and refining national reports to ensure they met global standards for data accuracy. These organizations worked alongside the Indira Gandhi Memorial Hospital, which serves as the national reference laboratory for validating test results. This partnership allowed the Maldives to use digital monitoring tools such as the Electronic Immunization Registry to track children’s health status in real time.
Promoting Equity With the Migrant Health Policy
The path to the Maldives’ historic triple elimination also involved ensuring that no resident was left behind due to background or legal status. The government recently launched a Migrant Health Policy that guarantees equal access to health services for all residents, including migrant populations. This inclusive policy reduced gaps in disease surveillance and ensured that every mother living in the country received the same standard of care. Experts note that including marginalized groups in national health frameworks is a critical factor in achieving disease elimination goals.
A Beacon of Hope for Global Health
The success of the Maldives serves as a beacon of hope for other nations working to eliminate preventable infections. By combining political leadership with a decentralized health system and strong international partnerships, the country has protected future generations from chronic disease. The Maldives’ historic triple elimination demonstrates that geographic isolation and resource constraints are not insurmountable barriers to public health progress. As countries move toward the 2030 global goal for triple elimination, the Maldives shows that equitable, high-quality health care can play a significant role in reducing poverty and improving lives.
– Elena Cárdenas
Elena is based in Monterrey, México and focuses on Global Health and Politics for The Borgen Project.
Photo: Flickr

 In 2023, about
In 2023, about 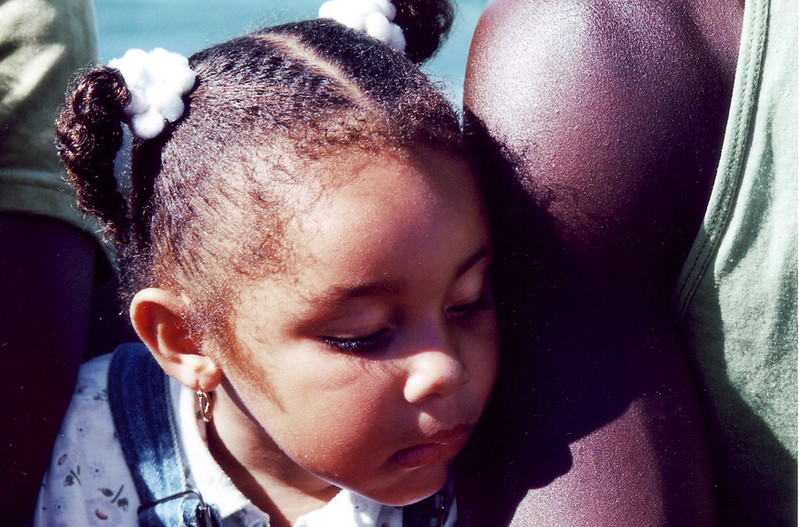 In May 2024, Belize achieved certification from the World Health Organization (WHO) for
In May 2024, Belize achieved certification from the World Health Organization (WHO) for 