
With its longevity and devastating effect on public health resources, the COVID-19 pandemic has strained access to healthcare, treatments and medications for other infectious diseases. Developing countries are particularly hit by this, where their progress in decreasing the numbers of HIV, malaria and tuberculosis are now at risk of a surge due to the lack of diagnostic tests and medicine available. The rise of COVID-19 has prompted countries and businesses alike to center their attention on mitigating the impact of the pandemic, disrupting global health supply chains. Without adequate funding and resources to treat these diseases as well, decades of progress will be undone, especially within poorer regions of the world.
Key Issues:
- The rise in COVID-19 has diminished health resources and treatment in other communicable diseases, like tuberculosis, HIV and malaria. Lockdowns and fear of catching COVID-19 has made it challenging for individuals fighting these diseases to access medication and receive diagnoses for their symptoms. This is especially amplified in poorer countries.
- Service delivery of treatments for tuberculosis, HIV and malaria have been cancelled or delayed due to the redirection of medical services to COVID-19. These disruptions could lead to an additional 500,000 deaths in HIV and 770,000 deaths from malaria.
- The Global Fund estimates that the death toll from these three infectious diseases could double by next year, reversing immense progress that has been made in mitigating the impact of these diseases due to the lack of detection, medication and resources.

Source: The Global Fund
Focus on Tuberculosis and COVID-19:
- Tuberculosis (TB) and COVID-19 are communicable diseases that critically impact the lungs. Both diseases exhibit similar symptoms, such as difficulty breathing, coughing, and an acute fever. However, their biggest difference lies in the incubation period and a slower onset. With these diseases exhibiting comparable effects, there is a risk that detection of TB will be harder to identify.
- Lack of TB detection is already prevalent in the four countries that typically account for the highest number of cases, namely India, Indonesia, the Philippines and South Africa. The World Health Organization (WHO) revealed that since the outbreak, there has been a massive drop in the reported number of TB cases.
- For example, India has about 27% of the world’s TB cases and diagnoses have dropped 75% with the onset of COVID-19.
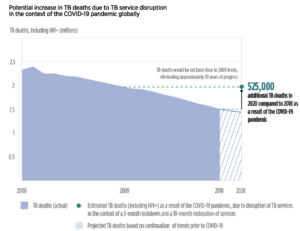
- WHO released a briefing outlining that 25% of TB detection will go unnoticed for three months as a result of the COVID-19 pandemic. Additionally, there will be a 13% increase in TB-related deaths worldwide.
- Lockdowns have the potential to lead to an additional 6.3 million cases of TB during the 2020-2025 period, which could lead to 1.4 million TB deaths.
- Moreover, the economic impact of the COVID-19 pandemic will exacerbate undernutrition and reduce incomes, resulting in a rise of TB cases. WHO estimates that there could be an increase of a million cases per year between 2020-2025.
- With the rising number of COVID-19 cases, services typically catered towards TB have been redirected towards mitigating the impact of COVID-19.
- WHO reported that there is increased social stigma against those who are perceived to have COVID-19. This has consequently discouraged individuals from seeking TB and COVID-19 treatments, undermining public health responses and social cohesion within communities.
Source: The Global Fund
The Borgen Project, Tuberculosis, and COVID-19:
In May 2020, The Borgen Project hosted a webinar discussion with Board Member Natalie Gill-Mensah, a global health programming expert, to explore the impact of COVID-19 on TB. Gill-Mensah leads teams that specialize in increasing TB treatment and diagnostics in low- and middle-income countries in Africa and Southeast Asia. Topics discussed in this webinar include the availability of TB services following the onset of COVID-19, the relationship between COVID-19 and TB detection, and the effect COVID-19 might have on TB drug resistance.
Support the End Tuberculosis Now Act:
To help take action against the rising number of TB cases at home and abroad, especially with the impact of COVID-19, email Congress to support the End Tuberculosis Now Act.
Steps Taken:
- Grants totaling up to $500 million and a COVID-19 Response Mechanism totaling up to $665 million from The Global Fund are currently being used to alleviate the effect of COVID-19 on HIV, TB and malaria disease programs and to ensure that countries are equipped with the medical resources to fight against all four of these infectious diseases.
- WHO has recommended that TB patients should receive pills instead of injections to help reduce travel to clinics during COVID-19 and guarantee access to proper treatment. Expanded prescriptions have also been applied to those with HIV.
- The Access to COVID-19 Tools (ACT) Accelerator brought together a variety of global health organizations, like the Bill & Melinda Gates Foundation and the World Bank, to ensure the equitable access and distribution of COVID-19 vaccines, tests, and treatment. This collaboration aims to reduce mortality and the severity of diseases, helping countries control the effects of COVID-19.
Urgent Action Needed:
- The Global Fund estimates that there needs to be an additional $5 billion to combat COVID-19 and ensure that access to TB, malaria and HIV treatment is secured in the midst of global supply chain disruptions in medication and diagnostic testing.
- Adequate distribution of personal protective equipment (PPE) among frontline health and community workers in poorer countries is needed to safeguard their health, especially since low-income countries pertain the lowest per capita ratio of health workers.
- Expand technological capacity to low- and middle-income countries to spark innovation in reinforcing laboratory diagnostic capabilities and to promote effective therapeutic techniques.
